Infertility is a complex and emotionally challenging journey that millions of individuals and couples worldwide face. From the initial realization of difficulty conceiving to exploring treatment options and confronting societal misconceptions, the road to parenthood can be fraught with uncertainties and obstacles. In this comprehensive guide, we delve into the intricacies of infertility, shedding light on its causes, exploring available treatment modalities, and dispelling common myths that surround it.
Understanding Infertility:
Infertility is defined as the inability to conceive after 12 months or more of regular, unprotected sexual intercourse, or after 6 months for women over 35. According to the World Health Organization (WHO), infertility affects an estimated 48.5 million couples worldwide. Despite its prevalence, infertility remains shrouded in stigma and misunderstanding, leading many to suffer in silence.
Causes of Infertility:
Infertility can stem from a myriad of factors, affecting both men and women. Let’s see a few major causes in men and women.
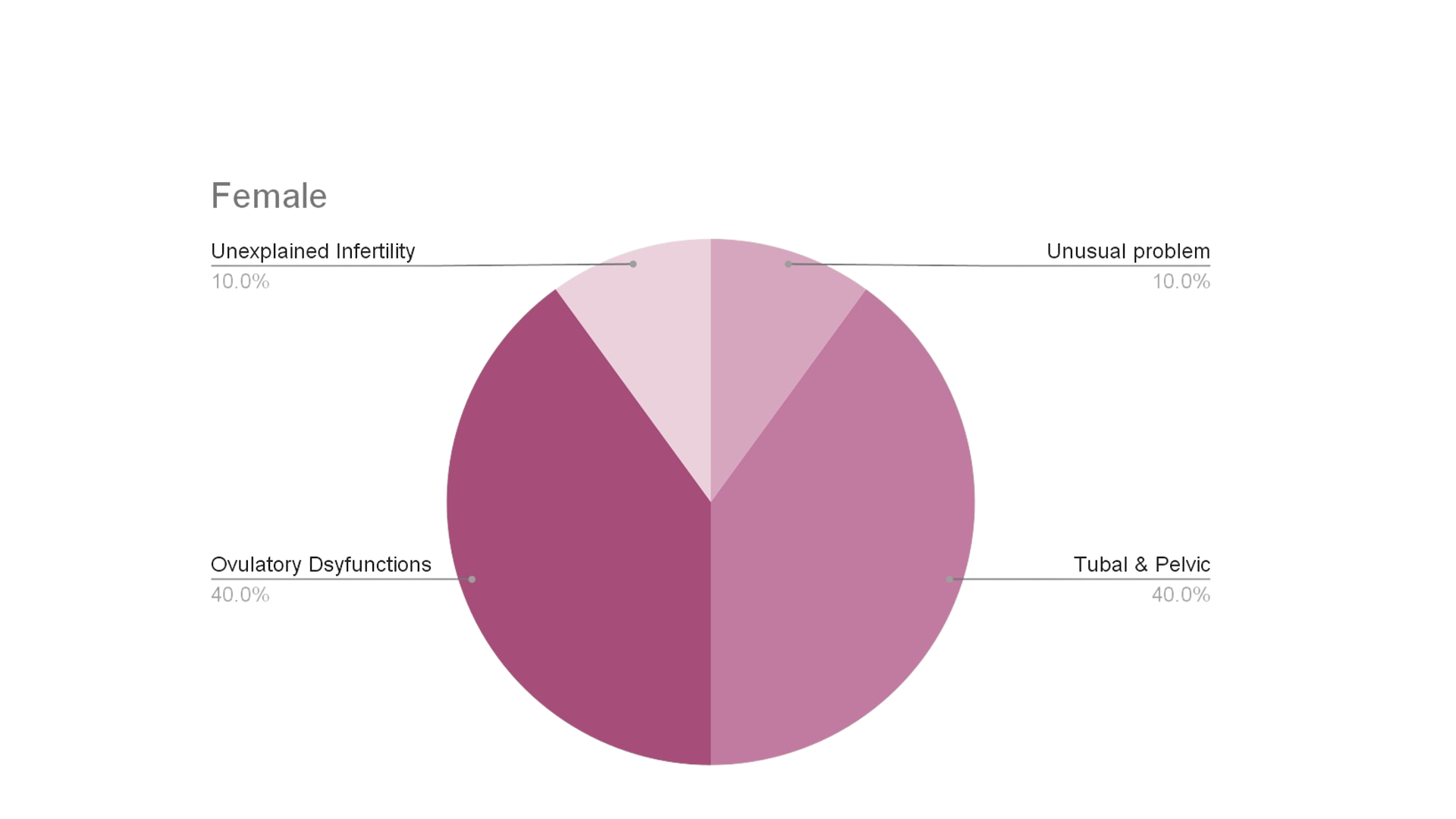
Causes of Infertility in Females:
A) Tubal & Pelvic Disorders:
Blocked Fallopian Tubes due to PID, STDs:
Pelvic Inflammatory Disease (PID) and sexually transmitted diseases (STDs) can cause inflammation and scarring in the fallopian tubes, preventing the egg from traveling to the uterus.
Endometriosis:
This condition occurs when tissue similar to the lining inside the uterus starts growing outside it, leading to inflammation, scarring, and blockages in the reproductive organs.
Pelvic Adhesions: Bands of scar tissue can form between pelvic organs after surgery, infection, or endometriosis, restricting their movement and functioning.
B) Uterine Causes:
Congenital Malformations:
Structural abnormalities in the uterus present from birth can hinder the implantation of an embryo or increase the risk of miscarriage.
Uterine Polyps:
These non-cancerous growths on the inner wall of the uterus can interfere with implantation or increase the risk of miscarriage.
Fibroids:
Benign tumors within the uterine wall can distort the shape of the uterus, causing blockages or altering the uterine environment.
Endometriosis:
As mentioned, endometriosis can affect the uterus, leading to scar tissue formation and other complications.
Asherman’s Syndrome:
Scar tissue or adhesions form inside the uterus, often due to surgical procedures, leading to a reduced uterine cavity.
C) Ovulatory Dysfunction:
PCOD (Polycystic Ovarian Disease):
This hormonal disorder affects the ovaries, leading to irregular menstrual cycles and ovulation issues.
Hyperprolactinemia:
Elevated levels of prolactin hormone can disrupt ovulation and menstrual cycles.
Hypo/Hyperthyroidism:
Both underactive and overactive thyroid glands can impact menstrual cycles and ovulation.
Eating Disorders:
Anorexia, bulimia, and other eating disorders can disrupt hormone levels and menstrual cycles.
Ovarian Tumors:
Tumors on the ovaries can interfere with their normal function and hormone production.
Primary Ovarian Insufficiency:
Often due to immune system disorders or genetic conditions like Turner syndrome, this leads to early menopause.
Radiation or Chemotherapy Treatment:
These cancer treatments can damage the ovaries, affecting their ability to function properly.
- D) Cervical Factors:
Cervical Stenosis:
A narrowing of the cervix can block sperm from entering the uterus.
Retroverted Uterus: Although generally not a direct cause of infertility, a tilted uterus can sometimes affect fertility.
Loss of Cervical Mucus:
Surgical procedures like amputation of the cervix, cone biopsies, or cervical diathermy can reduce or eliminate cervical mucus, which is essential for sperm transport.
Causes of Infertility in Males:
- Low Sperm Count, Low Motility, or Abnormal Sperm Shape:
Lifestyles:
Factors such as smoking, excessive alcohol consumption, and drug use can adversely affect sperm production and quality.
Hormones:
Imbalances in hormones such as testosterone can impact sperm production and function.
Health Factors:
Conditions like obesity, diabetes, and varicoceles (enlarged veins in the scrotum) can reduce sperm quality.
Genetic Issues:
Chromosomal abnormalities or genetic mutations can affect sperm production or function.
Stress & Anxiety:
Psychological stress can impact hormone levels and reduce sperm quality.
Physical Factors:
Injuries or surgeries affecting the reproductive organs can impair sperm production.
Infections: Infections in the reproductive tract, such as epididymitis or prostatitis, can damage sperm or reduce their quality.
Exploring Treatment Options:
The journey to overcoming infertility often involves a multifaceted approach tailored to individual needs and circumstances. For women, treatment options may include lifestyle modifications, such as maintaining a healthy weight and quitting smoking, medications to stimulate ovulation, and surgical interventions to address structural abnormalities. Similarly, men may benefit from lifestyle changes, hormone therapy, surgical procedures, or assisted reproductive technologies (ART) like intracytoplasmic sperm injection (ICSI) and varicocele repair.
Assisted Reproductive Technologies (ART):
In recent years, advancements in reproductive medicine have revolutionized the field of infertility treatment, offering hope to countless individuals and couples. Assisted reproductive technologies (ART), including in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and intrauterine insemination (IUI), have become increasingly accessible and effective in helping individuals achieve their dream of parenthood. According to the Centers for Disease Control and Prevention (CDC), ART accounts for over 99% of all assisted reproductive technology procedures in the United States [3].
Dispelling Myths:
Despite the growing awareness and acceptance of infertility as a medical condition, numerous myths and misconceptions persist in society. From blaming individuals for their inability to conceive to perpetuating harmful stereotypes, these myths can exacerbate the emotional toll of infertility and hinder access to appropriate care and support. It is essential to debunk these myths and foster a culture of empathy, understanding, and inclusivity for those navigating the challenges of infertility.
Here are a few common myths, let’s debunk them…
Myth 1: Infertility is Always a Woman’s Problem.
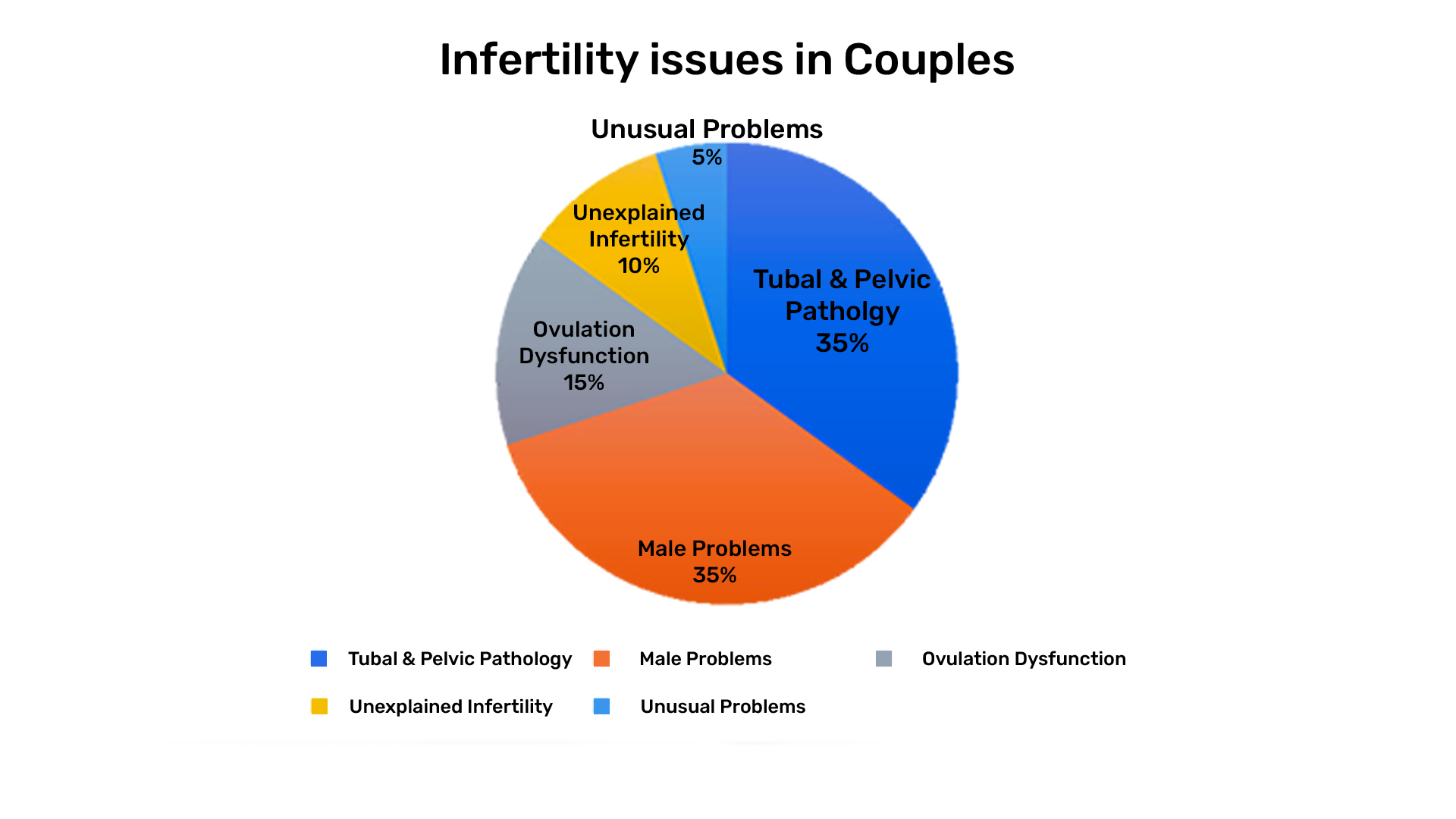
Infertility is a condition that affects both men and women equally. According to the American Society for Reproductive Medicine (ASRM), about one-third of infertility cases are attributed to female factors, one-third to male factors, and the remaining third to a combination of both or unexplained causes. Both partners should undergo evaluation to determine the cause of infertility.
Myth 2: Age Doesn’t Affect Men’s Fertility.
While women’s fertility declines more sharply with age, men are not immune to the effects of aging on fertility. Studies have shown that sperm quality and quantity can decrease with age, leading to lower fertility rates and higher risks of genetic abnormalities. It’s important for men to be aware that age can impact their reproductive health as well.
Myth 3: Infertility Means You’ll Never Have Children.
Infertility does not mean a permanent inability to have children. Many couples who experience infertility eventually conceive with the help of medical treatments such as IVF, IUI, or other assisted reproductive technologies. Lifestyle changes, medications, and surgical interventions can also improve fertility chances.
Myth 4: Stress Causes Infertility.
While stress can affect overall health and well-being, it is not a direct cause of infertility. However, the experience of infertility can be stressful and managing stress is important for overall health. Couples facing infertility should seek support and counseling to help manage stress and emotional strain.
Myth 5: You Should Try Harder, and It Will Happen.
Infertility is a medical condition that often requires more than just “trying harder.” Medical evaluation and treatment are essential for diagnosing and addressing underlying causes of infertility. Encouraging people to seek professional help rather than just trying harder can lead to better outcomes.
Myth 6: Once You Use IVF, You Will Definitely Get Pregnant
While IVF is a highly effective treatment for many, it does not guarantee pregnancy. Success rates vary based on factors such as age, underlying fertility issues, and overall health. It’s important for couples to have realistic expectations and to understand that multiple cycles may be necessary.
Myth 7: Lifestyle Factors Don’t Impact Fertility.
Lifestyle choices such as smoking, excessive alcohol consumption, poor diet, and lack of exercise can significantly impact fertility in both men and women. Encouraging healthy habits can improve fertility outcomes. For example, maintaining a healthy weight, eating a balanced diet, and avoiding harmful substances are all steps that can enhance reproductive health.
Myth 8: Infertility Treatments Are Always Expensive.
While some fertility treatments can be costly, there are various options and financial assistance programs available. It’s important to explore all options and consult with a fertility specialist about potential costs and financial support.
Myth 9: Birth Control Use Causes Infertility.
There is no evidence to suggest that using birth control causes infertility. Most women regain their fertility soon after stopping birth control. Long-term use of contraception does not impact a person’s ability to conceive in the future. If there are delays in conception after discontinuing birth control, other underlying issues should be investigated.
Myth 10: Infertility is Rare
Infertility is more common than many people realize. The World Health Organization (WHO) estimates that around 1 in 6 people globally experience infertility at some point in their reproductive lives. Raising awareness about the prevalence of infertility can help reduce stigma and encourage more people to seek help.
Conclusion:
Infertility is a journey fraught with uncertainty, but it is also one filled with hope, resilience, and courage. By understanding the underlying causes, exploring available treatment options, and dispelling common myths, we can empower individuals and couples to navigate their fertility journey with confidence and compassion. Together, we can break the silence surrounding infertility, support those in need, and celebrate the diversity of paths to parenthood. Remember, you are not alone, and there is always hope on the horizon.
References:
- World Health Organization. Infertility. Available at: [https://www.who.int/news-room/fact-sheets/detail/infertility]
- American Society for Reproductive Medicine. Infertility: An Overview. Available at: [https://www.asrm.org/topics/topics-index/infertility-an-overview/]
- Centers for Disease Control and Prevention. Assisted Reproductive Technology (ART). Available at: [https://www.cdc.gov/art/index.html]
